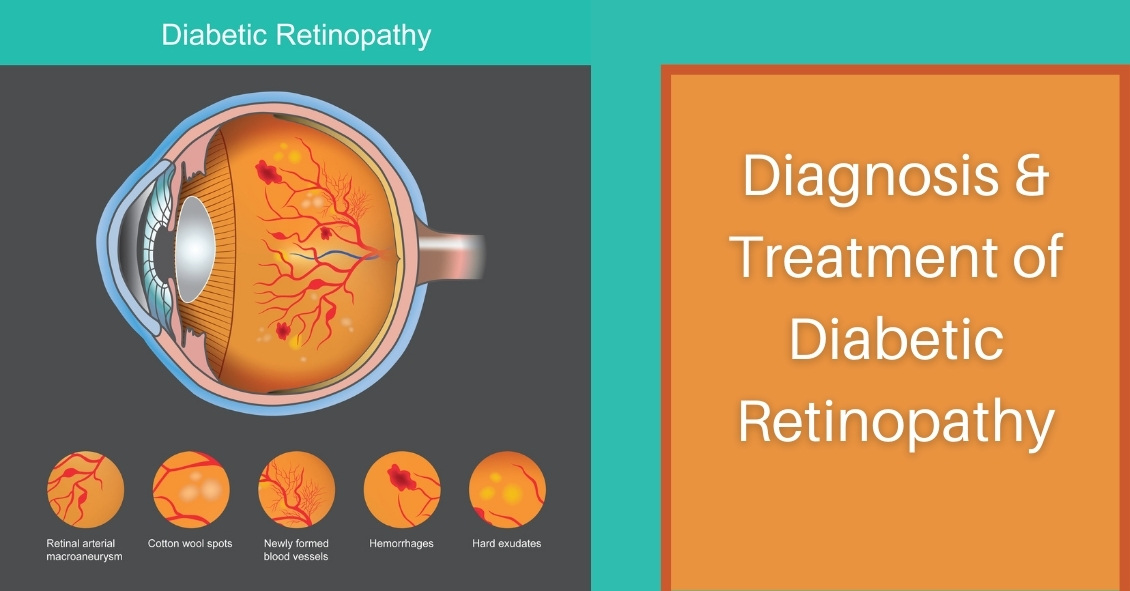
Diabetic retinopathy is an eye condition that can affect the retina of people who have diabetes.
The retina is the light-sensitive tissue that lines the back of the eye, and it detects light that is then processed as an image by the brain. Chronically high blood sugar or large fluctuations in blood sugar can damage the blood vessels in the retina. This can result in bleeding in the retina or leakage of fluid.
Diabetic retinopathy can be divided into non-proliferative or proliferative diabetic retinopathy.
Non-proliferative diabetic retinopathy: In the early stage of the disease, there is weakening of the blood vessels in the retina that causes out-pouching called microaneurysms. These microaneurysms can leak fluid into the retina. There can also be yellow deposits called hard exudates present in the retina from leaky vessels.
Diabetic macula edema is when the fluid leaks into the region of the retina called the macula. The macula is important for sharp, central vision needed for reading and driving. The accumulation of fluid in the macula causes blurry vision.
Proliferative diabetic retinopathy: As diabetic retinopathy progresses, new blood vessels grow on the surface of the retina. These blood vessels are fragile, which makes them likely to bleed into the vitreous, which is the clear gel that fills the middle of the eye. Bleeding inside the eye is seen as floaters or spots. Over time, scar tissue can then form on the surface of the retina and contract, leading to a retinal detachment. This is similar to wallpaper contracting and peeling away from the wall. If left untreated, retinal detachment can lead to loss of vision.
Symptoms of diabetic retinopathy:
- Asymptomatic: In the early stages of mild non-proliferative diabetic retinopathy, the person will usually have no visual complaints. Therefore, it is important for people with diabetes to have a comprehensive dilated exam by their eye doctor once a year.
- Floaters: This is usually from bleeding into the vitreous cavity from proliferative diabetic retinopathy.
- Blurred vision: This can be the result of fluid leaking into the retina, causing diabetic macular edema.
Risk factors for diabetic retinopathy:
- Blood sugar. Lower blood sugar will delay the onset and slow the progression of diabetic retinopathy. Chronically high blood sugar and the longer the duration of diabetes, the more likely chance of that person having diabetic retinopathy.
- Medical conditions. People with high blood pressure and high cholesterol are at greater risk for developing diabetic retinopathy.
- Ethnicity. Hispanics, African Americans, and Native Americans are at greater risk for developing diabetic retinopathy.
- Pregnancy. Women with diabetes could have an increased risk of developing diabetic retinopathy during pregnancy. If they already have diabetic retinopathy, it might worsen during pregnancy.
Article contributed by Jane Pan M.D.
This blog provides general information and discussion about eye health and related subjects. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately licensed physician. The content of this blog cannot be reproduced or duplicated without the express written consent of Eye IQ.